Part 3 of Safe Supply Saves Lives: a look beyond the deadly war on drugs, a 7-part series.
For many chronic pain patients, the result of a singular regulatory focus on reducing prescribing has been tragic. Amanda Votta has had rheumatoid arthritis for over 30 years, and the debilitating pain of bone grinding is only relieved with opioids. After the 2016 CDC guidelines came out, her doctors suddenly discontinued her prescription.1Stone, Will. “CDC Weighs New Opioid Prescribing Guidelines amid Controversy over Old Ones.” NPR, April 9, 2022, sec. Treatments. https://www.npr.org/sections/health-shots/2022/04/09/1091689867/opioid-prescribing-guidelines-pain. Finding a new provider willing to still prescribe in this environment was difficult. Earlier this year, 20,000 pain patients in California faced the same crisis when a private clinic chain suddenly shut down due to an investigation into Medicaid billing fraud for ordering excessive tests.2Barry-Jester, Anna Maria, and Jenny Gold. “‘Injections, Injections’: Troubling Questions Follow Closure of Big Pain Clinic Chain.” Los Angeles Times, February 22, 2022. https://www.latimes.com/california/story/2022-02-22/troubling-questions-follow-closure-big-pain-clinic-chain. One such patient, Audrey Audelo Ramirez, told the Kaiser Health News that she called, “every pain management clinic in Fresno,” and none were taking new patients. The LA Times-published report found that “many practices have rules against taking new patients on opioids, or will refuse to prescribe doses above certain thresholds.”
We know that when you stop prescribing opioids, some people end up with death from suicide, overdose, increased illicit opioid use, pain exacerbations. It’s really important to have a continuity, and that is not really possible in the current opioid-prescribing culture.
Dr. Phillip Coffin, director of substance abuse research for the San Francisco Department of Public Health

Doctors have a reason to be fearful, Drug Enforcement Administration warrants will cite the CDC guidelines as evidence of overprescribing. Providers targeted by authorities for having overprescribed are often handed fines over $100,000, lose their medical licensing and can face criminal charges.3Drug Enforcement Administration. “Doctor Pays $153,000 to Resolve Allegations of Overprescribing Opioids at His Escondido Clinic,” December 11, 2020. https://www.dea.gov/press-releases/2020/12/11/doctor-pays-153000-resolve-allegations-overprescribing-opioids-his.4Jordan and Miller. “Feds: 12 Charged for over-Prescribing Opioids, Including in Kentucky and Ohio.” WCPO 9 Cincinnati, May 4, 2022. https://www.wcpo.com/news/local-news/feds-12-charged-for-over-prescribing-opioids-including-in-kentucky-and-ohio. Doctors are held personally responsible because a patient lied to them and sold their medication. The experience of severe pain is personal and the diagnosis is qualitative; expecting doctors to serve as perfect lie detectors threatens their ability to adequately care for their patients. States and hospitals have accepted that outcome and taken discretion away from the provider. Each US state has established Prescription Drug Monitoring Programs to automatically enforce the guidelines and cap prescriptions. Most use the Narx Score, a product of private contractor Bamboo Health that uses a proprietary algorithm to assign every US resident an addiction risk score based on private health information. History of illicit substance use is one of many factors that can make it impossible for patients to be prescribed opioids, regardless of medical indication.

Four days into being hospitalized for uterine cysts, 32-year-old endometriosis patient Kathryn was suddenly denied care and accused of “drug seeking” when doctors saw her NarxCare score.6Szalavitz, Maia. “The Pain Was Unbearable. So Why Did Doctors Turn Her Away?” Wired, August 11, 2021. https://www.wired.com/story/opioid-drug-addiction-algorithm-chronic-pain/. Her gynecologist quickly followed in terminating care, again citing the NarxCare score. Kathryn later found out the score had been inflated by her elderly dog’s medications, which are counted under the owner’s name as a red flag. Women disproportionately receive high scores, and the score is especially hard on patients with disabilities or chronic illness.
40-year–old Nita Enyeart was quickly diagnosed with a kidney stone after getting to the hospital, but was denied the standard course of pain medication when they checked her NarxCare score. Nita reported that the nurse’s demeanor suddenly changed, telling her, “We saw your score and saw that you were trying to seek drugs.” Seeing multiple specialists for complex medical conditions is read in the algorithm as likely “drug shopping,” assuming that a patient is going from doctor to doctor until one will prescribe a desired recreational medication.
As Undoing Drugs author Maia Szalavitz describes, these unaccountable scores are not just a piece of advice for doctors, but can also serve as a legal threat, with dubious privacy standards:
Appriss [since rebranded as Bamboo Health] is adamant that a NarxCare score is not meant to supplant a doctor’s diagnosis. But physicians ignore these numbers at their peril. Nearly every state now uses Appriss software to manage its prescription drug monitoring programs, and most legally require physicians and pharmacists to consult them when prescribing controlled substances, on penalty of losing their license. In some states, police and federal law enforcement officers can also access this highly sensitive medical information—in many cases without a warrant—to prosecute both doctors and patients.
Under-prescribing pain relief medicine is all too familiar for Black Americans and attempts to further filter who is prescribed them will only exacerbate the existing racial inequality. In a 2016 study, half of medical students and residents held the false belief that Black people have a higher biological pain tolerance than white people.7Hoffman et al. “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences between Blacks and Whites.” Proceedings of the National Academy of Sciences 113, no. 16 (April 19, 2016): 4296–4301. https://doi.org/10.1073/pnas.1516047113. This trope is rooted in centuries of medical racism where Black Americans have been dehumanized to justify exploiting as test subjects. Steep discrepancies in pain medication prescribing have been found by race for treating children with appendicitis8Goyal et al. “Racial Disparities in Pain Management of Children With Appendicitis in Emergency Departments.” JAMA Pediatrics 169, no. 11 (November 2015): 996–1002. https://doi.org/10.1001/jamapediatrics.2015.1915. and adults with metastatic and recurrent cancers.9Anderson, Karen O., Carmen R. Green, and Richard Payne. “Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care.” The Journal of Pain 10, no. 12 (December 1, 2009): 1187–1204. https://doi.org/10.1016/j.jpain.2009.10.002.
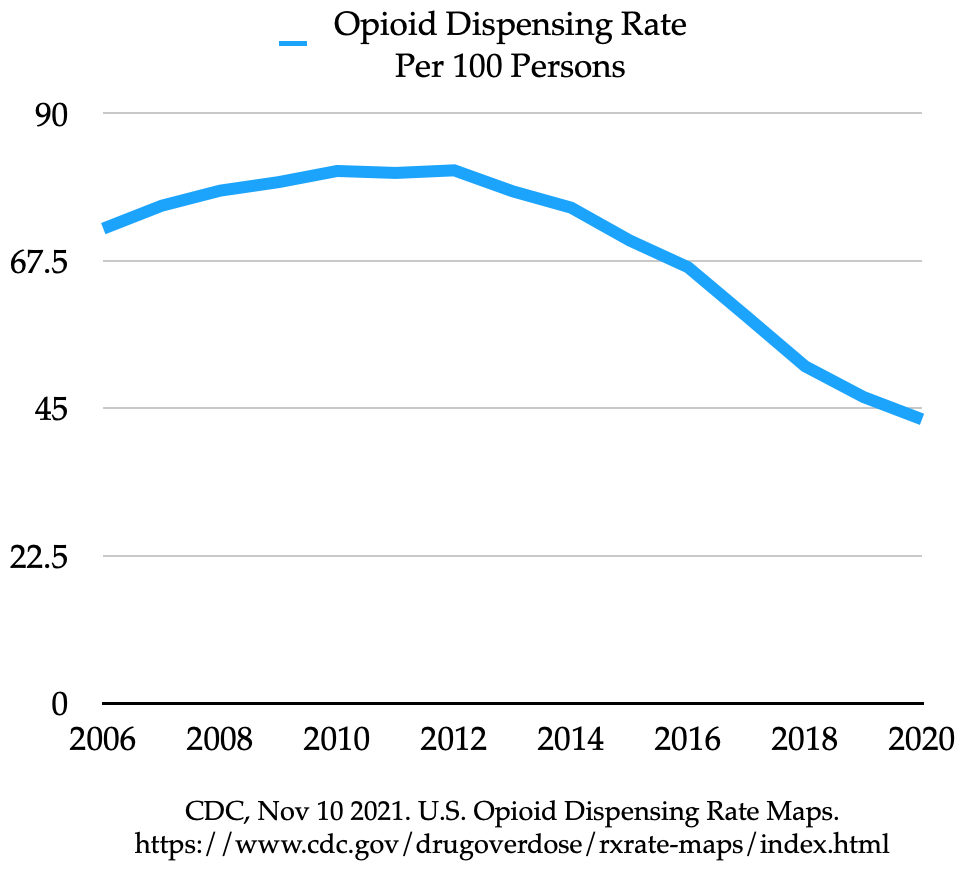
The US and its medical industry have made it harder than ever to get legitimate medication in the name of preventing addiction, but legitimate medication is not driving the overdose crisis. Just 13,503 of those 108,000 deaths involved pharmaceutical-grade opioids, let alone being used by the person prescribed them.10CDC. “U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020 – But Are Still Up 15%,” May 11, 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm. The regulatory system sees chronic pain patients as “addicts” due to their physical dependence in tolerance and withdrawal symptoms, even when the treatment is necessary to maintain their quality of life. It does not apply this same standard to the many other medications that garner physical dependence, such as anti-depressants, insulin, or blood pressure medication.
Journalist Zachary Siegal gives an apt summary of the past ten years:
The main action taken—aside from run of the mill drug war law enforcement—was to tighten the prescription opioid supply. It was a simple logic: less pills, means less addiction, means less deaths. The only problem is: the complete fucking opposite thing happened. Clamping down on pills led to heroin which led to fentanyl which led to obscene death rates on a scale we’ve never seen before.11Siegel, Zachary. “How the US Drug Supply Became an Ungodly Synthetic Cocktail of Death.” Substack newsletter. Substance (blog), April 5, 2022. https://tanag.substack.com/p/how-the-us-drug-supply-became-an.
The CDC has said that its 2016 guidance was misinterpreted, intending to be considered contextually rather than applied as rigidly as medical, insurance, and legislative authorities took it. The CDC slightly loosened its most specific guidelines in 2022, and emphasized that opioids do have a place. However, individual US states have set enforceable dose and duration maximums, and it’s hard to imagine going back.12Vestal, Christine. “States Likely to Resist CDC Proposal Easing Opioid Access.” The PEW Charitable Trust, March 1, 2022. https://pew.org/3sxOMHt. Florida is one such state, and their Department of Health has already disavowed the CDC for recognizing opioids as essential medication, citing Hulu’s DopeSick series in their press release.13“Now Is Not the Time for the CDC to Relax Opioid Prescription Guidelines.” Florida Department of Health, November 22, 2022. https://www.floridahealth.gov/newsroom/2022/11/20221122-cdc-relax-opioid-guidelines.pr.html.
Chronic pain patients and their effective care plans have been disregarded in a misguided war against prescribing. They’ve been pigeonholed as “drug seeking” with a substance use disorder, and the result is illicit and dangerous self-medicating, not “recovery.” Politicians have inserted themselves between doctors and patients, rejecting the expertise, lived experience, and diagnostic justification of both in favor of severing treatment because a television show made it popular. The CDC’s revisions indicate the relentless advocacy of patients struggling under this regime is making an impact. However, the DEA and state-level enforcement will not acquiesce in harming patients anytime soon.
Continue reading in Defining Substance Use Disorder and Addiction Remission
References
- 1Stone, Will. “CDC Weighs New Opioid Prescribing Guidelines amid Controversy over Old Ones.” NPR, April 9, 2022, sec. Treatments. https://www.npr.org/sections/health-shots/2022/04/09/1091689867/opioid-prescribing-guidelines-pain.
- 2Barry-Jester, Anna Maria, and Jenny Gold. “‘Injections, Injections’: Troubling Questions Follow Closure of Big Pain Clinic Chain.” Los Angeles Times, February 22, 2022. https://www.latimes.com/california/story/2022-02-22/troubling-questions-follow-closure-big-pain-clinic-chain.
- 3Drug Enforcement Administration. “Doctor Pays $153,000 to Resolve Allegations of Overprescribing Opioids at His Escondido Clinic,” December 11, 2020. https://www.dea.gov/press-releases/2020/12/11/doctor-pays-153000-resolve-allegations-overprescribing-opioids-his.
- 4Jordan and Miller. “Feds: 12 Charged for over-Prescribing Opioids, Including in Kentucky and Ohio.” WCPO 9 Cincinnati, May 4, 2022. https://www.wcpo.com/news/local-news/feds-12-charged-for-over-prescribing-opioids-including-in-kentucky-and-ohio.
- 5NarxCare Support Center. “What Is a Narx Score? How Is It Calculated?” Accessed December 5, 2022. https://narxcare.zendesk.com/hc/en-us/articles/4409648586899-What-Is-a-Narx-Score-How-Is-It-Calculated-.
- 6Szalavitz, Maia. “The Pain Was Unbearable. So Why Did Doctors Turn Her Away?” Wired, August 11, 2021. https://www.wired.com/story/opioid-drug-addiction-algorithm-chronic-pain/.
- 7Hoffman et al. “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences between Blacks and Whites.” Proceedings of the National Academy of Sciences 113, no. 16 (April 19, 2016): 4296–4301. https://doi.org/10.1073/pnas.1516047113.
- 8Goyal et al. “Racial Disparities in Pain Management of Children With Appendicitis in Emergency Departments.” JAMA Pediatrics 169, no. 11 (November 2015): 996–1002. https://doi.org/10.1001/jamapediatrics.2015.1915.
- 9Anderson, Karen O., Carmen R. Green, and Richard Payne. “Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care.” The Journal of Pain 10, no. 12 (December 1, 2009): 1187–1204. https://doi.org/10.1016/j.jpain.2009.10.002.
- 10CDC. “U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020 – But Are Still Up 15%,” May 11, 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm.
- 11Siegel, Zachary. “How the US Drug Supply Became an Ungodly Synthetic Cocktail of Death.” Substack newsletter. Substance (blog), April 5, 2022. https://tanag.substack.com/p/how-the-us-drug-supply-became-an.
- 12Vestal, Christine. “States Likely to Resist CDC Proposal Easing Opioid Access.” The PEW Charitable Trust, March 1, 2022. https://pew.org/3sxOMHt.
- 13“Now Is Not the Time for the CDC to Relax Opioid Prescription Guidelines.” Florida Department of Health, November 22, 2022. https://www.floridahealth.gov/newsroom/2022/11/20221122-cdc-relax-opioid-guidelines.pr.html.