Part 6 of Safe Supply Saves Lives: a look beyond the deadly war on drugs, a 7-part series.
History of Safe Supply in the US
An apt comparison to a safe supply of substances is legal alcohol and its own history of prohibition. Since 1933, people with alcohol use disorder have had access to a regulated and labeled supply so that they know the exact dose they’re consuming. They won’t die from the possibility of random amounts of methanol ending up in their product, and licensed safe consumption sites (‘bars’) are publicly available that have a legal responsibility to prevent overdose. The availability of safe alcohol is essential; liquor stores remained open globally during COVID-19 lockdowns, with governments acknowledging the harm of forced withdrawal was riskier than the virus.1Priest, Max Jordan Nguemeni Tiako, Kelsey C. “Yes, Liquor Stores Are Essential Businesses.” Scientific American Blog Network, April 7, 2020. https://blogs.scientificamerican.com/observations/yes-liquor-stores-are-essential-businesses/. Most people post-prohibition agree that this regulation and safe supply does not “enable” the genuine harm that chronic alcohol use causes, but rather it allows people to live to the day that they can take their own path of recovery.

Few safe supply advocates would employ the same regime currently used for alcohol with all drugs. Laissez-faire marketing regulations allow alcohol to maintain its cultural grip despite growing evidence that no amount of alcohol can be regularly consumed without some level of cumulative harm.3Raphelson, Samantha. “No Amount Of Alcohol Is Good For Your Health, Global Study Says.” NPR, August 24, 2018, sec. Health. https://www.npr.org/2018/08/24/641618937/no-amount-of-alcohol-is-good-for-your-health-global-study-claims. Establishing capitalistic enterprises for opioids and amphetamines the same way we’ve done with cannabis – which demands infinite market growth – is not the only option to deliver safe supply. Vancouver’s Drug User Liberation Front (DULF) hopes to see the Compassion Club model legalized for all drugs, and has applied for authorization to do just that.4DULF. “Evaluative Compassion Club Framework.” July 4 2022. Accessed December 3, 2022. https://www.dulf.ca/framework. Medical cannabis compassion clubs are non-profit, cooperative organizations where patients internally grow and share cannabis. Without legal authorization, DULF has applied their proposal by obtaining methamphetamine, heroin, and cocaine from the Dark Web, thoroughly testing it for dosing and contents before packaging and giving it away for free during political demonstrations.5Moakley, Paul. “The ‘Safe Supply’ Movement Aims to Curb Drug Deaths Linked to the Opioid Crisis.” Time, October 25, 2021. https://time.com/6108812/drug-deaths-safe-supply-opioids/.

Across the history of regimes, governments have promoted, allowed or criminalized the use of coffee, tobacco, alcohol, cannabis, psilocybin, opioids, and cocaine. In 17th Century Ottoman Empire, for example, alcohol was prohibited and coffee distribution could garner the death penalty, but cannabis and opium were permissible.7Szalavitz, Maia. Undoing Drugs: How Harm Reduction Is Changing the Future of Drugs and Addiction. Hachette, 2021. LOC 111/567. The legal status of substances has never been a consistent reading of best-known health risk factors, it’s been to serve certain political, and often racist, goals.

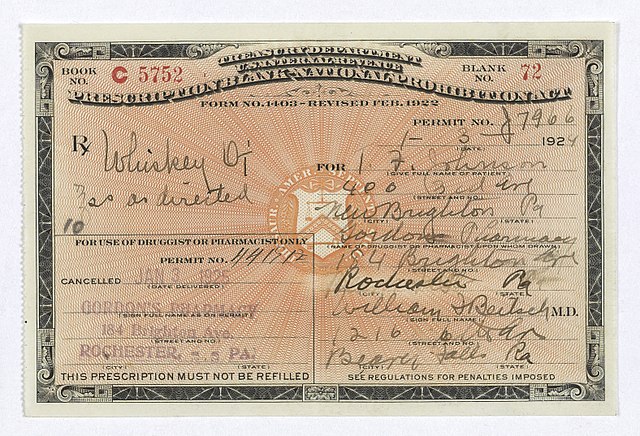
In the US, cannabis, morphine, heroin and cocaine were famously available home remedies from the late 18th century to 1910s, a time before any FDA regulation of medication. The US began its drug war with the Harrison Narcotics Tax Act of 1914, but initially, doctors were able to prescribe these newly controlled substances for the purpose of maintenance.9Blanchard, Sessi Kuwabara. “What We Can Learn From Harm Reduction’s Defeats,” February 15, 2022. https://www.thenation.com/article/culture/maia-szalavitz-undoing-drugs/. People dependent on substances could continue to use them under the monitoring of a medical professional. Today we would call this harm reduction through safe supply, or Heroin-Assisted Treatment. The socially constructed distinction between “drugs” and “medicine” had not yet been drawn, and there was still an acknowledged medical benefit to not dying from unregulated supply or being forced to suffer withdrawal symptoms. In an era of temperance, this practice made it to the Supreme Court by 1919. In Webb v. United States, familiarly, the Court played Doctor and ruled that maintaining the “comfort” of a habitual user was not a “legitimate medical purpose.” Now, you’re either a “patient prescribed medicine from a doctor” or an “addict peddled dope from a dealer.” The last narcotic maintenance program in the US closed in 1923.
Safe Supply In Practice
In the United Kingdom, no formal end to narcotic maintenance was mandated. The government even explicitly endorsed maintenance medication in a 1926 report. Negative media attention during the counterculture movement lead up to a 1984 Thatcher policy that advised a shift towards the US abstinence-only model, at which point clinics were largely forced to taper patients off of even methadone.10Szalavitz, Maia. Undoing Drugs: How Harm Reduction Is Changing the Future of Drugs and Addiction. Hachette, 2021. LOC 72/567. Still, the mechanism for safe supply had not been abolished. The Halton Drug Dependency Clinic in Liverpool was one straggling clinic that had never ended safe supply funded by the NHS, and when Dr. John Marks took over the practice at the dawn of the HIV outbreak, he recognized that patients prescribed heroin for decades on end were living well-adjusted lives and were not at risk of contracting HIV.11Ibid. LOC 59/567. The Halton clinic was remarkably ahead of its time in harm reduction, encouraging that patients switch to smokable forms of heroin instead of intravenous, a tactic the wider movement has taken up in the past decade. In 1995, a glowing 60 Minutes special highlighted the clinic’s success, but drew scrutiny from the Clinton-era US administration, who pressured its tragic shutdown.12Ibid. LOC 357/567 When one patient was asked by 60 Minutes “Why give addicts drugs?” she answered, “So they have a chance to live, like everyone else does. No one would hesitate to give other sorts of maintaining drugs – to diabetics who need insulin- in my mind it’s no different, I need heroin to live.”13Rx Drugs. 60 Minutes (US). Liverpool, UK, 1995. https://www.youtube.com/watch?v=Zy_86iVhmkQ. Within two years of closure, 25 of Dr. Marks’ 450 patients had died.14Gray, Mike. “Success Is Unacceptable If It’s Not Our Way.” Los Angeles Times, August 26, 1998. https://www.latimes.com/archives/la-xpm-1998-aug-26-me-16618-story.html. Individual patients who had recovered to stable and gainful lives while on a safe supply returned to homelessness and chaotic use of street drugs.
In their 1976 decision to decriminalize cannabis, officials in The Netherlands understood that criminalization was the cause of harm in cannabis use: the illicit market exposes customers to other illegal goods, including “hard drugs.” 15Ibid. LOC 68/567 Activist drug users recognized the ills of prohibition could not be solved with cannabis alone. In response to a Hepatitis B outbreak among injection drug users, the Rotterdam Junkiebond (Junkie’s Union) established the world’s first syringe exchange program in 1981, before HIV had even been identified. 16Ibid. LOC 69/567 The approach was soon adopted – with much political opposition – by organizers fighting the HIV outbreak in Tacoma, New York, California, and elsewhere, and was synthesized with the safe supply work in Liverpool to constitute Harm Reduction.

Switzerland became the first country to launch a Heroin-Assisted Treatment clinical trial in 1994. With the trial showing quick success, HAT became a regularly available treatment option across Switzerland by 1999. Annual mortality rates for illicit drug users in Switzerland had been 2.5-3% in the 1990s. Swiss HAT patients from 1994-2000 carried an annual mortality rate of just 1.1%.17Rehm, Jürgen, Ulrich Frick, Christina Hartwig, Felix Gutzwiller, Patrick Gschwend, and Ambros Uchtenhagen. “Mortality in Heroin-Assisted Treatment in Switzerland 1994-2000.” Drug and Alcohol Dependence 79, no. 2 (August 1, 2005): 137–43. https://doi.org/10.1016/j.drugalcdep.2005.01.005. Even then, the leading cause of death among HAT participants was from HIV/AIDS. In all such cases, HIV infection had occurred prior to entering HAT: if harm reduction methods had been deployed sooner, those deaths could have also been prevented. Following Switzerland’s rollout of Heroin-Assisted Treatment, per capita drug-related deaths fell from 5.3 per 100,000 to 1.6 per 100,000.18Swiss Health Observatory. “Drug-Related Deaths,” August 29, 2022. https://ind.obsan.admin.ch/en/indicator/monam/drug-related-deaths. Prior to HAT, Swiss were dying from drugs at nearly double the rate of Americans. In 2021 Switzerland’s drug-related death rate was just 1/20th that of the US.
A two-year randomized controlled trial of 515 HAT patients in Germany found that, “HAT is associated with improvements in mental and physical health in the long term.”19Verthein, Uwe, Karin Bonorden-Kleij, Peter Degkwitz, Christoph Dilg, Wilfried K. Köhler, Torsten Passie, Michael Soyka, Sabine Tanger, Mario Vogel, and Christian Haasen. “Long-Term Effects of Heroin-Assisted Treatment in Germany.” Addiction (Abingdon, England) 103, no. 6 (June 2008): 960–66; discussion 967-968. https://doi.org/10.1111/j.1360-0443.2008.02185.x. HAT is now a standard treatment option in much of Northern Europe, where street fentanyl remains unheard of.
The North American Opiate Medication Initiative (NAOMI) was a landmark randomized controlled trial administering the first Heroin-Assisted Treatment (HAT) pilot in Canada from 2005-2008.20Oviedo-Joekes, Eugenia, Bohdan Nosyk, Suzanne Brissette, Jill Chettiar, Pascal Schneeberger, David C. Marsh, Michael Krausz, Aslam Anis, and Martin T. Schechter. “The North American Opiate Medication Initiative (NAOMI): Profile of Participants in North America’s First Trial of Heroin-Assisted Treatment.” Journal of Urban Health : Bulletin of the New York Academy of Medicine 85, no. 6 (November 2008): 812–25. https://doi.org/10.1007/s11524-008-9312-9. Chronic opioid users who had experienced at least three unsuccessful attempts at treatment (including one attempt at methadone) were recruited. The majority of study participants were in Vancouver’s Downtown Eastside, with 73% homeless or unstably housed. 111 participants received a standard course of methadone, while 115 were intravenously dosed heroin under medical supervision up to three times per day. Patients prescribed heroin had the option to switch to oral methadone at any point in the study, and 20% did.
NAOMI researchers found that the HAT group was associated with a greater reduction in criminal activity and better treatment retention. The heroin group, “had greater improvements with respect to medical and psychiatric status, economic status, employment situation, and family and social relations,” than the methadone group. The only death in the trial occurred in the methadone group from an outside illicit opioid overdose. Overall, however, heroin presented as causing more medical risks. Zero adverse events were associated with the methadone prescription, while the HAT group experienced 24 adverse medical events attributed to the treatment, including non-fatal overdoses and seizures. NAOMI offers a strong basis that while HAT does not eliminate medical risks, it can be more effective than methadone at stabilizing people’s lives and offers a lower chance of patients returning to street drugs. Despite the success of HAT in NAOMI, efforts to implement safe supply in Canada were paused until the 2020s.
Canada has authorized a variety of safe supply pilot programs in the last 3 years, but they’ve lacked the scale necessary to reach a meaningful number of users the way Switzerland was able to. They typically fail to meet clients where they’re at by expecting people to immediately switch to different forms of opioids and amphetamines, drawing a line based on the stigma attached to a particular drug’s name. The doses of Dilaudid that most safe supply patients are prescribed often barely touch their fentanyl tolerance. Victoria BC’s SAFER, an outreach case management program serving unsheltered adults, initially only had the authorization to prescribe hydromorphone under its safe supply pilot, which they found was not relevant to daily fentanyl users. That’s started to change in the past year. Since 2021, SAFER has gained access to prescribe three forms of fentanyl, to be consumed under medical supervision.21Medrano, Kastalia. “A BC Safe Supply Program Pushes the Medical Model as Far as It Will Go.” Filter (blog), February 3, 2022. https://filtermag.org/medical-safe-supply-fentanyl/. Vancouver permanent supportive housing non-profit PHS started North America’s first take-home safe supply fentanyl program.22Johnson, Doug. “Vancouver Safe Supply Program Begins Prescribing Take-Home Fentanyl.” Filter (blog), April 13, 2022. https://filtermag.org/safe-supply-phs-vancouver-prescription-fentanyl/. Aiming to fully replace rather than supplement a user’s illicit drug consumption, PHS charges participants a market rate of $10 per take-away dose. Pilots in BC also offer stimulant MAT, a practice absent from the US, by prescribing Ritalin and Adderall. The scale remains wholly insufficient, with patient numbers in the low hundreds in a region with tens of thousands of illicit opioid and methamphetamine users.
The data clearly shows a medical use cases for Heroin-Assisted Treatment; it has measurable benefits and drawbacks compared to methadone and Suboxone treatments. Patients should have the right to make an informed decision on the best treatment plan for them with their doctor, but right now that’s possible. Law enforcement agencies and the Supreme Court should have no role in deeming evidence-based medical treatments illegal. If regulators have any interest in actually solving the overdose crisis, they ought to stop blocking what we know works.
Continue reading in Reducing Harm is the Right’s New Culture War Target
References
- 1Priest, Max Jordan Nguemeni Tiako, Kelsey C. “Yes, Liquor Stores Are Essential Businesses.” Scientific American Blog Network, April 7, 2020. https://blogs.scientificamerican.com/observations/yes-liquor-stores-are-essential-businesses/.
- 2Library of Congress, Washington, D.C. 20540 USA. “Labor Unions Hold Anti-Prohibition Meeting.” Image, October 31, 1931. https://www.loc.gov/item/99405158/.
- 3Raphelson, Samantha. “No Amount Of Alcohol Is Good For Your Health, Global Study Says.” NPR, August 24, 2018, sec. Health. https://www.npr.org/2018/08/24/641618937/no-amount-of-alcohol-is-good-for-your-health-global-study-claims.
- 4DULF. “Evaluative Compassion Club Framework.” July 4 2022. Accessed December 3, 2022. https://www.dulf.ca/framework.
- 5Moakley, Paul. “The ‘Safe Supply’ Movement Aims to Curb Drug Deaths Linked to the Opioid Crisis.” Time, October 25, 2021. https://time.com/6108812/drug-deaths-safe-supply-opioids/.
- 6The American Magazine Vol.124 No. 1 July 1937 ‘”Marihuana: The Assassin of Youth” infographic sponsored by Consolidated Brewer’s Association of America. The American Magazine Vol.124 No. 1 July 1937
- 7Szalavitz, Maia. Undoing Drugs: How Harm Reduction Is Changing the Future of Drugs and Addiction. Hachette, 2021. LOC 111/567.
- 8Infrogmation of New Orleans. Commercially Marketed Heroin Containers from the Early 20th Century. Bottle on Left; Box on Right. The Box Has a “Harrison Act” Tax Stamp, Indicating a Date of 1914 or Shortly after. Photographed from Display at the Old Mint Museum, New Orleans. Photographed 2010. Photo by Infrogmation. https://commons.wikimedia.org/wiki/File:HeroinHarrisonActNOLA.JPG.
- 9Blanchard, Sessi Kuwabara. “What We Can Learn From Harm Reduction’s Defeats,” February 15, 2022. https://www.thenation.com/article/culture/maia-szalavitz-undoing-drugs/.
- 10Szalavitz, Maia. Undoing Drugs: How Harm Reduction Is Changing the Future of Drugs and Addiction. Hachette, 2021. LOC 72/567.
- 11Ibid. LOC 59/567.
- 12Ibid. LOC 357/567
- 13Rx Drugs. 60 Minutes (US). Liverpool, UK, 1995. https://www.youtube.com/watch?v=Zy_86iVhmkQ.
- 14Gray, Mike. “Success Is Unacceptable If It’s Not Our Way.” Los Angeles Times, August 26, 1998. https://www.latimes.com/archives/la-xpm-1998-aug-26-me-16618-story.html.
- 15Ibid. LOC 68/567
- 16Ibid. LOC 69/567
- 17Rehm, Jürgen, Ulrich Frick, Christina Hartwig, Felix Gutzwiller, Patrick Gschwend, and Ambros Uchtenhagen. “Mortality in Heroin-Assisted Treatment in Switzerland 1994-2000.” Drug and Alcohol Dependence 79, no. 2 (August 1, 2005): 137–43. https://doi.org/10.1016/j.drugalcdep.2005.01.005.
- 18Swiss Health Observatory. “Drug-Related Deaths,” August 29, 2022. https://ind.obsan.admin.ch/en/indicator/monam/drug-related-deaths.
- 19Verthein, Uwe, Karin Bonorden-Kleij, Peter Degkwitz, Christoph Dilg, Wilfried K. Köhler, Torsten Passie, Michael Soyka, Sabine Tanger, Mario Vogel, and Christian Haasen. “Long-Term Effects of Heroin-Assisted Treatment in Germany.” Addiction (Abingdon, England) 103, no. 6 (June 2008): 960–66; discussion 967-968. https://doi.org/10.1111/j.1360-0443.2008.02185.x.
- 20Oviedo-Joekes, Eugenia, Bohdan Nosyk, Suzanne Brissette, Jill Chettiar, Pascal Schneeberger, David C. Marsh, Michael Krausz, Aslam Anis, and Martin T. Schechter. “The North American Opiate Medication Initiative (NAOMI): Profile of Participants in North America’s First Trial of Heroin-Assisted Treatment.” Journal of Urban Health : Bulletin of the New York Academy of Medicine 85, no. 6 (November 2008): 812–25. https://doi.org/10.1007/s11524-008-9312-9.
- 21Medrano, Kastalia. “A BC Safe Supply Program Pushes the Medical Model as Far as It Will Go.” Filter (blog), February 3, 2022. https://filtermag.org/medical-safe-supply-fentanyl/.
- 22Johnson, Doug. “Vancouver Safe Supply Program Begins Prescribing Take-Home Fentanyl.” Filter (blog), April 13, 2022. https://filtermag.org/safe-supply-phs-vancouver-prescription-fentanyl/.